Table of Contents
Fentanyl Stay in your System
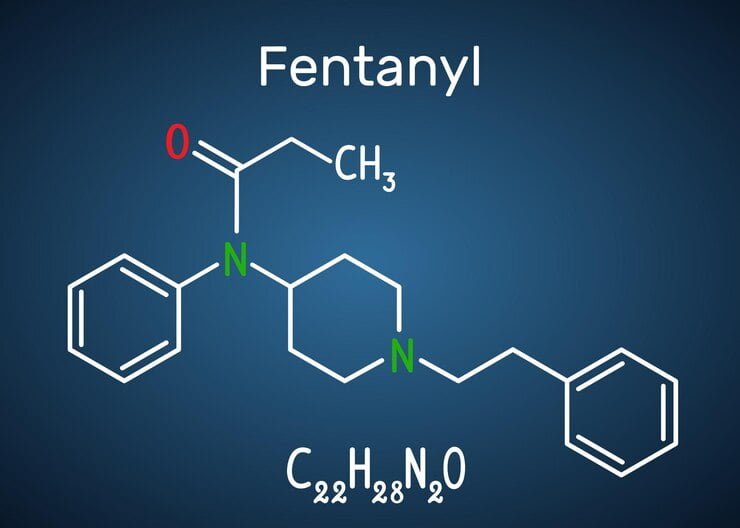
Fentanyl is a powerful synthetic opioid that is used to manage severe pain but is also known for its high potential for abuse and overdose. One of the most frequently asked questions about fentanyl is, “How long does fentanyl stay in your system?” This is a crucial factor for patients, healthcare providers, and those undergoing drug testing.

Understanding the pharmacokinetics of fentanyl, including its metabolism, half-life, and how it is detected in the body, helps provide a clear picture of how long the drug remains in your system.
Introduction to Fentanyl Metabolism
Fentanyl is metabolized primarily by the liver, where it is broken down into inactive metabolites. Once administered, fentanyl rapidly enters the bloodstream and binds to opioid receptors, providing pain relief but also leading to potential side effects and risks. The duration for which fentanyl stays in your system depends on several factors, including the form of fentanyl, the dosage, and individual metabolic rates.
Factors Affecting How Long Fentanyl Stays in Your System
Several factors influence how long fentanyl remains in your body:
- Dosage: Higher doses of fentanyl take longer to be eliminated from the body.
- Frequency of Use: Chronic use of fentanyl can lead to accumulation in the body, prolonging its detection time.
- Form of Fentanyl: Fentanyl can be administered via injections, patches, lozenges, or nasal sprays. Transdermal patches, for example, provide a slow release of fentanyl, causing it to remain in the system for a longer duration than a single injection.
- Individual Factors: Metabolism, body fat percentage, age, hydration level, and liver function all impact how long fentanyl stays in the system.
- Health Conditions: People with compromised liver or kidney function may metabolize fentanyl more slowly, prolonging its presence in the body.
Fentanyl Half-Life
The half-life of a drug refers to the amount of time it takes for half of the drug to be eliminated from the bloodstream. Fentanyl has a relatively short half-life, but it varies depending on how the drug is administered.
- Intravenous Fentanyl: The half-life is between 2 to 4 hours.
- Transdermal Patches: The half-life is much longer, usually around 17 hours, due to the slow release of the drug into the bloodstream over time.
However, just because the half-life is short doesn’t mean fentanyl leaves the system quickly. It can still be detectable in different parts of the body for extended periods, especially with chronic use.
How Long Fentanyl is Detectable in the Body
The detection window for fentanyl varies based on the type of drug test used. Different parts of the body, such as blood, urine, saliva, and hair, will retain traces of fentanyl for different amounts of time.
Blood
Fentanyl is detectable in the blood for about 5 to 48 hours after the last dose. Blood tests are often used in clinical settings for acute cases, as fentanyl clears from the bloodstream relatively quickly.
Urine
Urine tests are more commonly used for drug screening, and fentanyl can typically be detected in urine for 24 to 72 hours after the last use. However, for people who use fentanyl chronically or in high doses, it can remain detectable in urine for up to 96 hours or more.
Saliva
Fentanyl is detectable in saliva for 1 to 4 days after use, depending on factors like dosage and individual metabolism. Saliva testing is less common but can be a useful method for detecting recent use of fentanyl.
Hair
Hair tests can detect fentanyl use for the longest duration—up to 3 months or even longer. This is because traces of fentanyl and its metabolites are deposited into hair follicles, providing a long-term record of drug use. Hair testing is typically used in forensic settings or for individuals undergoing long-term drug monitoring.
How Fentanyl is Metabolized
Fentanyl is primarily metabolized by the CYP3A4 enzyme in the liver, which converts it into nor-fentanyl, an inactive metabolite. Both fentanyl and nor-fentanyl are then excreted through urine. The speed of this metabolic process can vary significantly between individuals due to genetic differences, liver function, and other health factors.
The drug’s short half-life means it is rapidly broken down, but chronic use can lead to a buildup of fentanyl in fatty tissues, prolonging the overall time it stays in the system. This is especially true with transdermal patches, which slowly release the drug over an extended period, causing it to linger in the body even after the patch is removed.
What is Fentanyl? A Comprehensive Guide
Fentanyl is a powerful synthetic opioid used primarily in medical settings to treat severe pain. It is considered one of the most potent pain relievers available and is approximately 50 to 100 times stronger than morphine. While it has legitimate medical uses, fentanyl is also associated with significant risks, including addiction and overdose, especially when misused.
Introduction to Fentanyl
Fentanyl is a Schedule II controlled substance, meaning it has a high potential for abuse but is also used for medical purposes under strict regulation. Developed in the 1960s, it quickly became a key pain management tool for patients suffering from chronic pain, post-surgical pain, or advanced cancer. However, its misuse has contributed to the rising opioid crisis, especially in North America.
How Does Fentanyl Work?
Fentanyl works by binding to opioid receptors in the brain and spinal cord, which regulate pain and emotions. Once it binds to these receptors, it blocks the transmission of pain signals and creates a feeling of euphoria, which can lead to misuse. Because of its potency, even small doses can provide significant pain relief, but they also increase the risk of addiction and overdose.
Medical Uses of Fentanyl
In clinical settings, fentanyl is prescribed for the management of severe pain, often in cases where other opioids, such as morphine, have failed. It is commonly used in:
- Post-Surgical Pain: To manage intense pain after major surgeries.
- Cancer Pain: For patients with chronic, severe pain, particularly those who are opioid-tolerant.
- Anesthesia: Fentanyl is sometimes used as part of anesthesia to help patients manage pain during and after surgery.
Forms of Fentanyl
Fentanyl comes in several forms for different medical applications:
- Injectable Fentanyl: Used in hospitals to manage acute pain during surgeries or emergencies.
- Transdermal Patches: These patches release fentanyl gradually over 72 hours, providing long-term pain relief for patients with chronic pain.
- Lozenges and Tablets: Used for breakthrough pain, especially in cancer patients.
- Nasal Sprays and Lollipops: These are fast-acting forms of fentanyl, offering quick relief for severe pain episodes.
Fentanyl Abuse and Risks
While fentanyl has legitimate medical uses, it is also widely abused due to its potent effects. Illicitly manufactured fentanyl has become a significant issue, often mixed with other drugs like heroin, cocaine, or methamphetamine, which increases the risk of overdose. A tiny amount of fentanyl, even as small as 2 milligrams, can be deadly.
Risks of Fentanyl Abuse:
- Addiction: Fentanyl is highly addictive due to the intense euphoria it can produce.
- Overdose: Because of its potency, it is easy to accidentally overdose on fentanyl, leading to respiratory depression and death.
- Illicit Use: Street versions of fentanyl, often in the form of powders, counterfeit pills, or mixed into other drugs, are extremely dangerous.
Fentanyl and the Opioid Crisis
Fentanyl has become one of the most significant contributors to the opioid crisis. In the U.S. and other parts of the world, fentanyl-related overdose deaths have surged in recent years. The primary reason is the illicit manufacturing and distribution of fentanyl, often in counterfeit pills or mixed with other substances without the user’s knowledge.
In 2020, synthetic opioids like fentanyl were involved in nearly 60% of all opioid overdose deaths in the United States, highlighting its deadly impact. Efforts to control the spread of illicit fentanyl include stricter regulations and improved access to treatments like naloxone (Narcan), which can reverse opioid overdoses if administered in time.
Fentanyl Risks and Side Effects: A Comprehensive Overview
Fentanyl, a potent synthetic opioid, is widely used for pain management but also carries significant risks and potential side effects. While it can provide effective relief from severe pain, misuse or improper administration of fentanyl can result in serious health complications, including overdose and death. Understanding the risks and side effects of fentanyl is essential for patients, healthcare providers, and anyone who may come into contact with this powerful drug.
Introduction to Fentanyl Risks
Fentanyl is primarily used in medical settings to treat patients with severe or chronic pain. However, its potency—estimated to be 50 to 100 times stronger than morphine—makes it one of the most dangerous opioids when misused. Even in therapeutic settings, fentanyl can lead to a range of side effects, from mild to life-threatening. This article provides a detailed look at the risks and side effects associated with fentanyl use.
Common Side Effects of Fentanyl
Like many opioids, fentanyl can cause a variety of side effects. These may occur even when the drug is taken as prescribed and under medical supervision.
Common Side Effects Include:
- Drowsiness and Fatigue: Fentanyl can make users feel extremely tired or lethargic, making it dangerous to operate heavy machinery or drive.
- Nausea and Vomiting: Gastrointestinal issues are common, particularly in those new to fentanyl use.
- Constipation: Fentanyl, like other opioids, can slow down the digestive system, often leading to chronic constipation.
- Dizziness and Lightheadedness: Some users may experience dizziness, especially when standing up quickly.
- Dry Mouth: Fentanyl can reduce saliva production, leading to a persistent dry mouth.
- Confusion: Mental clouding, memory issues, and confusion can occur, particularly in older patients.
- Sweating: Excessive sweating is another common side effect of fentanyl.
While these side effects are not typically life-threatening, they can significantly affect quality of life and may require medical attention if they persist.
Serious Side Effects and Risks
Fentanyl is associated with several more severe side effects, particularly when misused or taken in excessive doses. These include:
- Respiratory Depression: Fentanyl can severely slow or stop breathing, particularly in high doses or in individuals who are not opioid-tolerant. Respiratory depression is the leading cause of death in fentanyl overdoses.
- Low Blood Pressure: Fentanyl can cause a significant drop in blood pressure, leading to dizziness, fainting, or even shock in extreme cases.
- Bradycardia (Slow Heart Rate): Fentanyl can reduce heart rate, which may become life-threatening if the heart rate drops too low.
- Seizures: While rare, seizures have been reported in some patients using fentanyl.
- Allergic Reactions: Some individuals may experience severe allergic reactions to fentanyl, characterized by rash, itching, swelling, severe dizziness, or trouble breathing.
Fentanyl Overdose
Due to its extreme potency, the risk of overdose with fentanyl is significantly higher than with other opioids. Even small miscalculations in dosage can result in overdose, particularly with illicitly manufactured fentanyl, which is often mixed with other drugs like heroin or cocaine.
Signs of Fentanyl Overdose Include:
- Extreme Drowsiness: Difficulty staying awake or inability to wake up.
- Slow or Shallow Breathing: Respiratory depression is the most dangerous sign of fentanyl overdose.
- Blue Lips or Fingernails: A sign of oxygen deprivation.
- Loss of Consciousness: Fentanyl can cause users to slip into a coma or become unresponsive.
- Pinpoint Pupils: Constricted pupils are a hallmark of opioid overdose.
Overdose can be fatal if not treated immediately.Naloxone (Narcan) is an opioid antidote that can reverse fentanyl’s effects if administered in time, but due to fentanyl’s potency, multiple doses of naloxone may be required.
Fentanyl Addiction and Dependence
Fentanyl is highly addictive, and even short-term use can lead to physical and psychological dependence. Addiction occurs when a person becomes compulsively driven to use the drug, even when it is no longer medically necessary. Dependence means the body has adapted to the drug, and stopping its use abruptly can lead to withdrawal symptoms.
Symptoms of Fentanyl Withdrawal:
- Muscle and Joint Pain
- Anxiety and Restlessness
- Sweating
- Insomnia
- Diarrhea and Vomiting
- Rapid Heart Rate
Withdrawal from fentanyl is challenging and often requires medical assistance or a detox program.
Fentanyl Interaction with Other Drugs
Fentanyl can interact with various other medications and substances, leading to dangerous effects. Some of the most common interactions include:
- Alcohol: Combining fentanyl with alcohol can significantly increase the risk of respiratory depression and overdose.
- Benzodiazepines: Drugs like Xanax, Valium, or Klonopin can enhance fentanyl’s depressant effects on the central nervous system, heightening the risk of sedation, respiratory depression, and death.
- Antidepressants: Certain antidepressants can increase fentanyl levels in the body, raising the risk of side effects and overdose.
- Other Opioids: Mixing fentanyl with other opioids, whether prescribed or illicit, can lead to overdose much faster than taking either drug alone.
Patients should always inform their healthcare provider about all the medications and substances they are using to prevent dangerous drug interactions.
How to Safely Use Fentanyl
If prescribed fentanyl, it is essential to follow the dosage instructions carefully and to take the drug exactly as directed by a healthcare professional. Here are some safety tips:
- Never alter the dose without consulting a doctor.
- Do not mix with alcohol or other sedatives unless approved by a healthcare provider.
- Store fentanyl securely to prevent accidental use by others, especially children.
- Dispose of unused fentanyl properly to prevent misuse.
For those using fentanyl patches, it is essential to avoid exposing the patch to heat, such as heating pads or hot tubs, as this can cause the drug to be released too quickly, increasing the risk of overdose.
FAQ on Fentanyl
1. What is Fentanyl?
Fentanyl is a powerful synthetic opioid used to manage severe pain, often prescribed for chronic pain or post-surgical patients. It is about 50 to 100 times stronger than morphine and requires careful medical supervision.
2. How long does Fentanyl stay in your system?
The duration fentanyl remains in the body depends on several factors such as the method of use, individual metabolism, and body fat. Typically, fentanyl can be detected:
- In blood: Up to 48 hours
- In urine: 24 to 72 hours
- In hair: Up to 90 days
3. What are the common side effects of Fentanyl?
Common side effects include:
- Drowsiness
- Nausea and vomiting
- Constipation
- Dizziness
- Dry mouth
- Sweating
- Confusion
4. What are the serious risks of using Fentanyl?
Serious risks include:
- Respiratory depression (slow or stopped breathing)
- Low blood pressure
- Slow heart rate (bradycardia)
- Seizures
- Allergic reactions
- Overdose, which can be fatal
5. Can Fentanyl cause addiction?
Yes, fentanyl is highly addictive. Even short-term use can lead to physical dependence, and long-term use can result in addiction, characterized by compulsive use despite harmful consequences.
6. What are the signs of a Fentanyl overdose?
Signs of a fentanyl overdose include:
- Extreme drowsiness or inability to wake up
- Slow or shallow breathing
- Blue lips or fingernails
- Pinpoint pupils
- Loss of consciousness
7. What should I do in case of a Fentanyl overdose?
If you suspect someone is experiencing a fentanyl overdose, immediately call emergency services. Naloxone (Narcan) can reverse the effects of an overdose, but due to fentanyl’s potency, multiple doses may be needed.
8. Can Fentanyl interact with other drugs?
Yes, fentanyl can interact dangerously with other substances, especially:
- Alcohol
- Benzodiazepines (e.g., Xanax, Valium)
- Antidepressants
- Other opioids
These interactions can increase the risk of severe side effects, including overdose.
9. How should Fentanyl be used safely?
Fentanyl should only be used under medical supervision. Follow the prescribed dosage exactly, avoid mixing with alcohol or other sedatives, and store it securely away from children. For fentanyl patches, avoid exposing the patch to heat, which can cause rapid drug release and increase overdose risk.
10. What should I do if I want to stop using Fentanyl?
Do not stop fentanyl use suddenly without consulting a healthcare provider, as withdrawal symptoms can be severe. Gradual tapering under medical supervision is often required to manage withdrawal safely.
11. Is Fentanyl involved in the opioid crisis?
Yes, fentanyl, especially illicitly manufactured forms, has played a significant role in the opioid crisis due to its high potency and frequent involvement in overdose deaths. Public awareness and responsible use are key to preventing further fatalities.
Conclusion on Fentanyl: Fentanyl stay in your System, Risks, and Side Effects
Fentanyl is a potent synthetic opioid used primarily for managing severe pain, but its strength and fast-acting nature also make it highly dangerous when misused. Fentanyl can remain in the body for varying durations depending on the method of administration and individual factors such as metabolism, body fat, and frequency of use. Generally, fentanyl can be detected in blood for up to 48 hours, in urine for 24 to 72 hours, and in hair for up to 90 days. The extended presence of fentanyl in the system increases the risk of overdose, especially when combined with other substances like alcohol or benzodiazepines.
The drug’s potency—estimated to be 50 to 100 times stronger than morphine—places users at significant risk of serious side effects, including respiratory depression, bradycardia, and even death, particularly when doses are miscalculated or when taken without medical supervision. While fentanyl provides effective pain relief for those with legitimate medical needs, it also comes with common side effects such as drowsiness, nausea, and constipation, and more severe risks such as low blood pressure, seizures, and allergic reactions.
One of the most alarming risks associated with fentanyl is its potential for overdose. Even small amounts of fentanyl can cause life-threatening symptoms, including extreme drowsiness, slow or shallow breathing, and loss of consciousness. The presence of illicitly manufactured fentanyl in the illegal drug market, often mixed with other drugs like heroin or cocaine, has significantly contributed to the growing number of opioid-related deaths worldwide.
Additionally, fentanyl poses a high risk of addiction and dependence, leading to withdrawal symptoms such as muscle pain, anxiety, insomnia, and vomiting. For individuals attempting to discontinue use, withdrawal can be severe and typically requires medical intervention.
Ultimately, while fentanyl can be an essential tool for managing extreme pain, its risks are undeniable. Proper medical supervision is crucial to avoid misuse, addiction, and fatal outcomes. Public awareness about fentanyl’s dangers, particularly its interaction with other substances, is critical in preventing overdoses and mitigating the opioid crisis.
Understanding the full spectrum of fentanyl’s effects—from its duration in the body to its potentially life-threatening risks—can help individuals use this powerful drug safely and responsibly. Read more about your health


Your article helped me a lot, is there any more related content? Thanks!
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?