Table of Contents
What are symptoms causes and transmission of Mpox monkey pox
Mpox, formerly known as monkey pox, is a viral disease caused by the monkey pox virus. This virus belongs to the orthopox virus genus, which also includes variola virus (which causes smallpox), vaccinia virus (used in the smallpox vaccine), and cowpox virus.
Mpox,monkeypox, is a rare viral disease that is similar to smallpox but less severe. It is caused by the monkeypox virus, which belongs to the same family of viruses as the variola virus, the causative agent of smallpox. Although mpox is less deadly than smallpox, it is still a significant health concern, especially in regions where the virus is endemic.
As of 2024, Mpox (formerly known as monkeypox) continues to be a significant public health concern globally. While mpox is similar to smallpox, it is generally less severe but still requires serious attention due to its capacity for transmission and outbreaks. This detailed guide explores the symptoms, causes, and transmission of mpox, providing up-to-date information on this viral disease.

What is Mpox?
Mpox is an infectious disease caused by the monkeypox virus, which is part of the Orthopoxvirus genus in the Poxviridae family. The virus was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, which is how the disease got its name. The first human case of mpox was recorded in 1970 in the Democratic Republic of the Congo.
Mpox is primarily found in central and western African countries, particularly in regions close to tropical rainforests. However, cases have been reported outside of Africa, typically linked to international travel or imported animals.
Key Points:
- Mpox is caused by the monkeypox virus, related to the smallpox virus.
- The disease is rare and usually occurs in central and western Africa.
- Mpox is less severe than smallpox but still requires medical attention.
Important Facts About Mpox (Monkeypox)
1. Mpox Is a Viral Disease:
Mpox is caused by the monkeypox virus, a member of the orthopoxvirus family, closely related to smallpox. While it shares symptoms with smallpox, mpox is generally less severe.
2. Two Types of Mpox Virus:
There are two genetic clades of the monkeypox virus: the Central African (Congo Basin) clade, which is more severe, and the West African clade, which is less severe. The Central African clade has higher mortality rates and increased human-to-human transmission.
3. Human-to-Human Transmission:
Mpox spreads through direct contact with an infected person’s skin lesions, body fluids, respiratory droplets (from prolonged face-to-face contact), and contaminated objects like bedding, clothing, or towels.
4. Symptoms Can Be Severe:
Mpox symptoms include fever, headache, muscle aches, fatigue, and a distinctive rash that develops into fluid-filled blisters and scabs. Severe cases may result in complications like secondary infections, pneumonia, and, in rare instances, death.
5. Animal-to-Human Transmission Still Occurs:
Mpox was originally transmitted from infected animals, particularly rodents and monkeys, to humans. This can occur through handling infected animals, their blood, or consuming undercooked meat from these animals.
6. Endemic and Global Spread:
Historically, mpox has been endemic in Central and West Africa, but outbreaks have occurred globally in recent years, notably in Europe, North America, and Asia, prompting increased surveillance and control efforts.
7. Swollen Lymph Nodes Are a Key Symptom:
One distinguishing symptom of mpox, compared to similar diseases like smallpox or chickenpox, is swollen lymph nodes, which can occur in the neck, armpits, or groin.
8. Incubation Period:
After exposure, the incubation period for mpox ranges from 5 to 21 days, with symptoms typically appearing 7 to 14 days post-exposure.
9. Self-Limiting Disease:
Most mpox cases resolve on their own within 2 to 4 weeks. Supportive care such as pain management and hydration helps, but severe cases might require hospitalization.
10. Vaccination Can Prevent Mpox:
Vaccines originally developed for smallpox, like Jynneos (Imvamune/Imvanex), have proven effective in preventing mpox, especially in healthcare workers and those exposed to the virus. Vaccination post-exposure can also reduce the severity of the disease.
11. Prevention Through Hygiene and Avoidance:
Prevention includes avoiding contact with infected individuals or contaminated objects, practicing good hygiene, frequent handwashing, and, in endemic areas, avoiding contact with wild animals.
12. Antiviral Treatment for Severe Cases:
In some cases, the antiviral drug tecovirimat (TPOXX) may be used to treat severe mpox infections, particularly for those with weakened immune systems.
13. Mpox Is Not Classified as an STI:
While mpox can spread through close physical contact, including during sexual activity, it is not classified as a sexually transmitted infection (STI). It spreads through direct contact with skin lesions or body fluids.
14. Mpox Is Not As Contagious As COVID-19:
Mpox is less contagious than respiratory viruses like COVID-19. Transmission requires close physical contact, unlike airborne viruses which spread more easily in public settings.
15. Global Monitoring and Public Health Response:
With the rise in cases outside of Africa, global health organizations such as the WHO and CDC have intensified surveillance, promoted vaccination, and provided guidance for handling outbreaks to control its spread.
- Initial: The MPox virus was first identified in laboratory monkeys in 1958, hence the original name. The first human case was recorded in the Democratic Republic of Congo (DRC) in 1970.
How is Mpox Transmitted?
Mpox can be transmitted to humans through direct contact with the blood, bodily fluids, or skin lesions of infected animals, such as monkeys, squirrels, and rodents. Human-to-human transmission can also occur, though it is less common. Transmission between humans can happen through:
1. Direct Contact:
- Why It Happens: Direct contact with the lesions, blood, or body fluids of an infected person can lead to transmission.
- Prevention Tip: Avoid close physical contact with anyone showing symptoms of mpox, especially if they have visible skin lesions.
2. Respiratory Droplets:
- Why It Happens: Prolonged face-to-face contact with an infected person can result in the inhalation of respiratory droplets carrying the virus.
- Prevention Tip: Wearing masks and maintaining physical distance in crowded or enclosed spaces can reduce the risk of transmission.
3. Contaminated Objects:
- Why It Happens: The virus can survive on surfaces and objects, such as bedding or clothing, that have been in contact with an infected person or animal.
- Prevention Tip: Regularly disinfect surfaces and avoid sharing personal items with someone who is infected.
4. Animal Bites or Scratches:
- Why It Happens: Bites, scratches, or consumption of undercooked meat from infected animals can lead to the transmission of the virus.
- Prevention Tip: Avoid contact with wild animals and ensure that all meat is properly cooked before consumption.
5. Animal to Human:
- The virus can spread from animals to humans through direct contact with blood, body fluids, or skin or mucosal lesions of infected animals. In Africa, evidence of monkey pox virus infection has been found in many animals, including rope squirrels, tree squirrels, Gambian pouched rats, dormice, various species of monkeys, and others.
6. Human to Human:
- Human-to-human transmission occurs through respiratory secretions, skin lesions of an infected person, or close contact with recently contaminated objects. Transmission through respiratory droplets usually requires prolonged face-to-face contact.
7. Sexual Transmission:
- Recent outbreaks indicate that mpox can spread during sexual activity due to the close physical contact involved. Mpox lesions can develop in the genital area, increasing the risk of transmission through intimate contact. While it’s not classified as a sexually transmitted infection (STI), sexual networks have been identified as significant contributors to recent outbreaks.
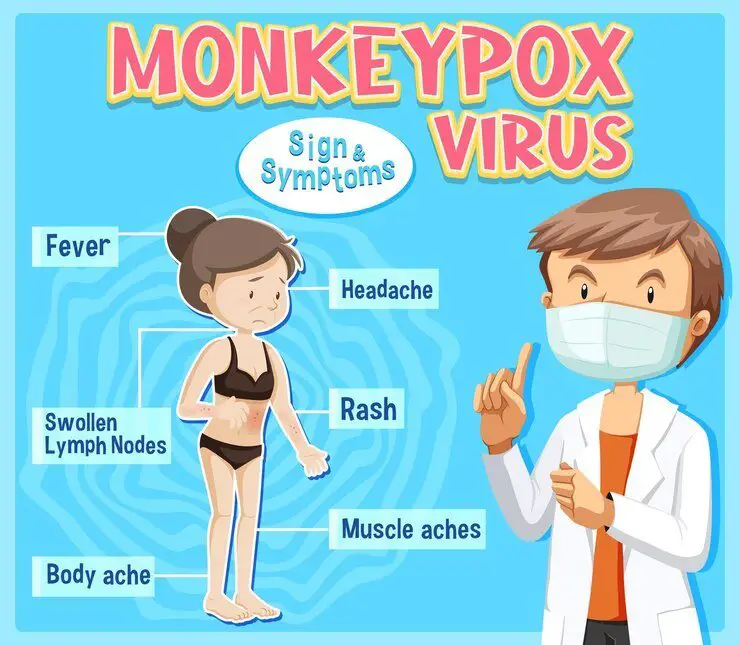
3. Symptoms of Mpox monkey pox :
The symptoms of mpox typically appear 5 to 21 days after exposure to the virus, with the illness lasting between 2 to 4 weeks. The symptoms are similar to those of smallpox but are generally milder. The disease progresses through several stages
Mpox Symptoms in 2024
Mpox symptoms are often mistaken for other viral infections at the onset, but its distinguishing rash and lesion progression set it apart. After exposure to the virus, symptoms usually develop within 5 to 21 days. The disease can last for 2 to 4 weeks, and it typically progresses through a series of stages.
Here are the most common symptoms of mpox in 2024:
- Fever: The onset of mpox often begins with a high fever, accompanied by chills and flu-like symptoms. This is one of the earliest indicators.
- Headache and Muscle Aches: Intense headaches and general body aches—especially in the back and muscles—are frequent and can persist through the early stages of infection.
- Swollen Lymph Nodes: Swollen lymph nodes in the neck, armpits, or groin are one of the telltale signs of mpox, distinguishing it from similar viral diseases like chickenpox or smallpox.
- Rash: A few days after the fever begins, a distinctive rash develops. It typically starts on the face and hands, and may spread to the rest of the body, including the palms, soles of the feet, and genital area. The rash progresses through several stages:
- Flat lesions (macules)
- Raised bumps (papules)
- Fluid-filled blisters (vesicles)
- Pus-filled sores (pustules)
- Scabs that eventually fall off.
- Fatigue: Patients may experience profound fatigue or exhaustion, often feeling extremely weak and unable to carry out daily tasks.
- Respiratory Symptoms: Some cases include cough, sore throat, and nasal congestion, particularly if the virus spreads through respiratory droplets in close contacts.
- The progression of the rash is a hallmark of mpox. The rash starts flat and eventually becomes raised and filled with fluid, turning into pus-filled sores that later scab over. The rash and lesions are often painful until the crusting stage, after which the healing process begins.
4. Severity of Mpox mokey pox:
The severity of mpox can vary significantly based on several factors, including the clade of the virus, individual health status, and the presence of underlying conditions. Here’s a detailed overview of the severity of mpox:
1. Clade Differences
- Central African (Congo Basin) Clade: This clade is associated with more severe disease and higher mortality rates, ranging from 1% to 10% in certain populations. The symptoms can be more pronounced, and complications are more common.
- West African Clade: Generally considered less severe, this clade has a lower mortality rate (approximately 1%). Infections from this strain typically result in milder symptoms and a better prognosis.
2. Clinical Symptoms
- Initial Symptoms: The disease often begins with flu-like symptoms such as fever, chills, headaches, and muscle aches, which can be distressing but are often manageable.
- Rash and Lesions: The characteristic rash, which can progress through several stages (macules, papules, vesicles, pustules, and scabs), can be painful and may lead to secondary infections, particularly in the skin.
- Swollen Lymph Nodes: The presence of swollen lymph nodes is a key symptom that can indicate a more severe infection.
3. Risk Factors for Severe Disease
Certain populations may be at a higher risk for severe outcomes, including:
- Immunocompromised Individuals: People with weakened immune systems (e.g., those with HIV/AIDS, cancer patients, or organ transplant recipients) are more susceptible to severe illness and complications.
- Young Children: Children, particularly those under 8 years of age, may be at higher risk of severe disease due to their developing immune systems.
- Pregnant Women: There is a potential risk for complications in pregnant women, including transmission to the fetus.
4. Complications
Severe mpox infections can lead to complications such as:
- Secondary Infections: Skin lesions can become infected, leading to additional health issues.
- Respiratory Issues: In some cases, mpox can lead to pneumonia or other respiratory complications.
- Scarring: The progression of the rash can result in significant scarring, particularly if lesions are not managed properly.
- Long-term Effects: While most recover fully, some individuals may experience long-term consequences, including scarring or psychological effects related to the disease’s severity and appearance.
5. Mortality Rate
- The overall mortality rate for mpox varies by clade:
- Central African Clade: Mortality can be as high as 10%, particularly in vulnerable populations.
- West African Clade: Mortality is significantly lower, averaging around 1%.
6. Treatment and Management
- Most cases of mpox are self-limiting, with symptoms resolving within 2 to 4 weeks. Supportive care, including pain management and hydration, is crucial.
- In severe cases, antiviral medications like tecovirimat (TPOXX) may be employed to manage the disease, particularly in high-risk patients.
7. Public Health Response
Early detection and public health interventions play a vital role in managing outbreaks and minimizing the severity of mpox cases. Vaccination strategies and education on prevention are essential components of controlling its spread.
In summary, While mpox is generally less severe than smallpox, it still poses significant health risks, particularly for certain populations. The disease can lead to severe symptoms and complications, and understanding its severity is crucial for effective prevention, early detection, and management. Ongoing public health efforts and research are essential to reduce the burden of mpox globally.
5. Treatment and Prevention Mpox monkey pox :
Mpox can be challenging to diagnose because its symptoms are similar to those of other illnesses, such as smallpox, chickenpox, and measles. Laboratory tests, including polymerase chain reaction (PCR) and blood tests, are used to confirm the presence of the monkeypox virus.
Mpox Prevention in 2024
To prevent the spread of mpox, it’s essential to understand the risks and take necessary precautions:
- Avoid Close Contact with Infected Individuals: If someone shows signs of mpox, especially a rash or lesions, avoid close physical contact.
- Practice Good Hygiene: Wash hands regularly with soap and water or use an alcohol-based hand sanitizer, especially after contact with infected individuals or potentially contaminated objects.
- Avoid Touching Contaminated Objects: Do not share bedding, clothing, towels, or other personal items with someone who may be infected.
- Vaccination: In 2024, vaccines originally developed for smallpox have proven effective in preventing mpox. These vaccines are available for high-risk individuals and healthcare workers. Jynneos (Imvamune) is one of the vaccines approved for preventing mpox.
- Safe Handling of Animals: If living in or traveling to endemic areas, avoid contact with wild animals that may carry the virus. Eating or handling bushmeat can increase the risk of infection.
Mpox Treatment in 2024
While there is no specific cure for mpox, most cases are self-limiting and resolve on their own within 2 to 4 weeks. However, supportive care and antiviral treatments can help manage severe cases:
- Symptomatic Treatment: Pain relievers, such as ibuprofen or acetaminophen, can be used to manage fever, headaches, and muscle aches. Proper hydration and rest are also essential for recovery.
- Isolation: Infected individuals should be isolated to prevent spreading the virus to others.
- Antiviral Medication: In more severe cases, especially for those with weakened immune systems, antiviral drugs like tecovirimat (TPOXX) may be prescribed. This drug is specifically approved for treating orthopoxvirus infections, including mpox.
How Mpox Has Evolved in 2024
Since its initial identification in 1958, mpox has mostly remained in Central and West Africa. However, in recent years, the disease has spread to non-endemic countries, partly due to increased global travel and closer physical contact in densely populated areas. With more robust surveillance, improved vaccines, and better public awareness, health authorities have a greater ability to contain outbreaks, though challenges still remain, particularly in urban areas.
6. Global concern on Mpox monkey pox:
Outbreaks of mpox have been reported in various parts of the world, particularly in Central and West African countries. However, in recent years, outbreaks have occurred in non-endemic countries, raising concerns about its global spread.
7. Recent Developments on Mpox monkey pox:
Mpox (formerly known as monkey pox) has no specific treatment, but the disease is usually self-limiting, meaning that most people recover on their own without specific medical treatment. However, there are supportive treatments and some antiviral medications that can be used to manage the symptoms and complications of the disease.
Self-Limiting Nature of Mpox (Monkeypox)
Mpox, also known as monkeypox, is generally considered a self-limiting disease. This means that in most cases, the illness resolves on its own without the need for extensive medical treatment. Here’s what you need to know about the self-limiting nature of mpox:
What Does Self-Limiting Mean?
A self-limiting disease is one that tends to resolve naturally over time as the body’s immune system fights off the infection. In the case of mpox, most individuals will recover without specific antiviral treatment, as the virus runs its course.
Key Points:
- Duration: Mpox typically lasts between 2 to 4 weeks.
- Recovery: Most patients recover fully without the need for antiviral medications.
- Symptom Management: Treatment usually focuses on alleviating symptoms, such as fever and rash, rather than targeting the virus itself.
How Does the Body Fight Mpox?
When a person is infected with the monkeypox virus, their immune system responds by producing antibodies and activating immune cells to combat the virus. Over time, these immune responses help to eliminate the virus from the body.
- Immune Response: The body’s natural immune response is usually sufficient to clear the virus, especially in individuals with healthy immune systems.
- Symptom Resolution: As the immune system gains control over the virus, symptoms gradually improve. The fever subsides, the rash goes through its stages, and the skin begins to heal as the lesions crust over and fall off.
Complications and Exceptions
While mpox is self-limiting for most people, certain groups may be at higher risk of complications, including:
- Immunocompromised Individuals: People with weakened immune systems, such as those with HIV/AIDS, cancer patients, or individuals on immunosuppressive therapy, may experience a more severe course of the disease.
- Children and Pregnant Women: Young children and pregnant women are also more susceptible to complications from mpox.
- Secondary Infections: In some cases, skin lesions can become infected with bacteria, leading to secondary infections that require antibiotic treatment.
For the majority of people, mpox is a self-limiting illness that will resolve with supportive care, including rest, hydration, and symptom management. However, if symptoms worsen or if you belong to a high-risk group, it’s important to seek medical attention. Early intervention can help manage complications and ensure a smoother recovery. Understanding the self-limiting nature of mpox helps in managing expectations and promotes confidence in the body’s ability to fight off the virus.
Supportive Care Mpox monkey pox:
- Symptomatic treatment: Supportive care is essential in managing MPox symptoms. This includes treating fever, headache, and pain with over-the-counter medications such as acetaminophen or ibuprofen. Ensuring adequate hydration and nutrition is also important.
- Wound care: Proper care of skin wounds is very important to prevent secondary bacterial infection. This may include the use of antiseptic solutions and wound dressings.
Antiviral Treatment of Mpox monkey pox:
- Tecovirimat (TPOXX): Tecovirimat is an antiviral drug that was originally developed to treat smallpox but has been approved in some countries for the treatment of MPOX, especially during outbreaks. . It works by blocking the virus’ ability to spread within the body. Although it is not a cure, it can help reduce the severity and duration of symptoms.
- Cidofovir and Brincidofovir: These are other antiviral agents that have shown some effectiveness against orthopoxvirus in laboratory settings. They are usually used in more severe cases or for patients with weakened immune systems.
Vaccination for Mpox monkey pox:
- Precautionary Vaccination: Vaccination against smallpox (with vaccines such as ACAM2000 or Jynneos) has been found to be about 85% effective in preventing Mpox. This is especially useful for people who have been exposed to the virus or who are at high risk of contracting the virus. Although it does not cure an active infection, it can prevent the onset of the disease or reduce its severity.
Management of serious cases
- Hospitalization: Severe cases of MPox, especially in people with weakened immune systems, pregnant women, or young children, may require hospitalization. In such cases, close monitoring and advanced supportive care, including intravenous fluids and antibiotics for secondary infections, may be necessary.
Challenges and Complications of Mpox monkey pox:
- Complications: While most people recover completely, some may experience complications such as loss of vision due to secondary bacterial infection, bronchopneumonia, sepsis, encephalitis, or corneal infection. is These complications can be life-threatening and require intensive medical treatment.
- Long-term effects: Some individuals may experience long-term effects, such as scarring from skin lesions or, in rare cases, permanent symptoms that require medical attention.
Public Health Measures
- Isolation and Prevention: Controlling the spread of M.pox is critical to controlling the outbreak. Infected individuals are usually isolated to prevent transmission, and close contacts may be monitored and offered vaccination.
FAQ: Mpox (Monkeypox) Symptoms, Causes, and Transmission in 2024
1. What is Mpox (Monkeypox)?
Mpox (previously known as monkeypox) is a viral zoonotic disease caused by the monkeypox virus, which belongs to the orthopoxvirus family, the same family as the virus that causes smallpox. While mpox shares similarities with smallpox, it is generally less severe. The virus can spread from animals to humans and from person to person.
2. What are the common symptoms of Mpox in 2024?
Common symptoms of mpox include:
- Fever
- Headache
- Muscle aches and back pain
- Swollen lymph nodes
- Fatigue
- Rash that progresses through several stages: flat spots, raised bumps, fluid-filled blisters, pustules, and finally scabs
- In some cases, respiratory symptoms such as a sore throat and cough.
3. What causes Mpox?
Mpox is caused by the monkeypox virus, which is typically transmitted to humans from infected animals, particularly rodents, monkeys, and other wild animals. Human-to-human transmission occurs through direct contact with an infected person’s body fluids, skin lesions, or respiratory droplets during close contact.
4. How is Mpox transmitted?
Mpox spreads through:
- Direct contact with the rash, lesions, or body fluids of an infected person.
- Respiratory droplets during close face-to-face contact.
- Contaminated objects such as bedding, towels, and clothing that have come into contact with an infected person’s lesions.
- Sexual contact, due to close physical interaction and contact with sores or bodily fluids.
- Animal-to-human transmission through contact with infected animals, especially in regions where mpox is endemic.
5. How long does it take for Mpox symptoms to appear?
Mpox symptoms typically appear 5 to 21 days after exposure to the virus. The illness usually lasts for 2 to 4 weeks.
6. What is the main difference between Mpox and smallpox?
While both mpox and smallpox are caused by viruses from the orthopoxvirus family, mpox is generally less severe than smallpox. Mpox also causes swollen lymph nodes, a symptom not typically seen in smallpox patients. Additionally, smallpox was eradicated globally through vaccination, whereas mpox still occurs in outbreaks, especially in non-endemic regions.
7. Is Mpox contagious?
Yes, mpox is contagious and can spread through direct contact with an infected person’s lesions or body fluids, respiratory droplets during close contact, and contaminated objects. It is also transmissible through close physical contact, such as sexual activity.
8. How can I protect myself from Mpox?
To protect yourself from mpox:
- Avoid close contact with individuals who show signs of mpox (especially rashes or lesions).
- Practice good hand hygiene, regularly washing your hands with soap and water or using hand sanitizer.
- Avoid touching contaminated objects, such as bedding, clothing, or towels of infected individuals.
- Get vaccinated if you are in a high-risk group or have been exposed to mpox.
9. Is there a vaccine for Mpox?
Yes, vaccines originally developed for smallpox, such as Jynneos (Imvamune/Imvanex), have been shown to be effective in preventing mpox. These vaccines are especially recommended for healthcare workers, people exposed to the virus, and individuals in high-risk groups.
10. Can Mpox be treated?
There is no specific antiviral treatment for mpox, but supportive care can help manage symptoms. In more severe cases, antiviral drugs like tecovirimat (TPOXX) may be used. Most people recover without treatment within 2 to 4 weeks. Hospitalization may be required for complications or severe cases.
11. How can I tell if I have Mpox?
The most distinguishing feature of mpox is the rash, which starts as flat spots and progresses to blisters and pustules before scabbing over. Swollen lymph nodes, along with fever and muscle aches, are also characteristic signs of mpox. If you suspect you have mpox, seek medical attention for testing and diagnosis.
12. How does Mpox spread through sexual contact?
While mpox is not classified as a sexually transmitted infection (STI), it can spread through intimate contact, including sexual activity. The close skin-to-skin interaction involved in sexual activity can lead to the transmission of the virus, particularly when rashes or lesions are present on the body or in the genital area.
13. What should I do if I think I have been exposed to Mpox?
If you believe you have been exposed to mpox:
- Isolate yourself to avoid spreading the virus to others.
- Contact a healthcare provider to discuss your symptoms and possible testing.
- Consider getting the mpox vaccine, especially if you’ve had direct contact with someone who has mpox.
14. How is Mpox diagnosed?
Mpox is diagnosed through a combination of clinical examination and laboratory testing. A doctor will assess your symptoms, particularly the rash and swollen lymph nodes, and may take samples from skin lesions for laboratory analysis to confirm the presence of the monkeypox virus.
15. Is Mpox still a concern in 2024?
Yes, mpox remains a concern in 2024 due to continued outbreaks in various regions. While vaccines and public health measures have helped reduce the spread, it is still important to be aware of the symptoms, transmission routes, and preventive strategies.
16. How severe is Mpox compared to other viral diseases?
Mpox is generally less severe than smallpox but can still cause significant illness, especially in immunocompromised individuals, children, or people with underlying health conditions. Most people recover within a few weeks, but severe cases may result in complications, including secondary infections, pneumonia, or scarring from the lesions.
17. What regions are at the highest risk for Mpox outbreaks?
Mpox has historically been endemic in Central and West Africa, but recent outbreaks have occurred in non-endemic regions, including parts of Europe, North America, and Asia. In densely populated areas or regions with close physical contact, the virus can spread more easily.
18. Can Mpox lead to long-term health effects?
In most cases, individuals fully recover from mpox without long-term effects. However, some individuals may experience scarring from the lesions, and rare complications such as secondary bacterial infections or respiratory issues can occur.
19. How can the spread of Mpox be controlled?
The spread of mpox can be controlled through:
- Isolation of infected individuals to prevent further transmission.
- Vaccination of high-risk groups and close contacts.
- Public awareness campaigns to educate people on how the virus spreads and how to protect themselves.
- Increased surveillance and early detection of outbreaks in at-risk regions.
20. What should communities do during a Mpox outbreak?
During a mpox outbreak, communities should:
- Encourage those showing symptoms to self-isolate and seek medical attention.
- Follow local public health guidelines for vaccination and preventive measures.
- Maintain good hygiene practices and avoid close contact with potentially infected individuals.
- Stay informed about the status of the outbreak and available healthcare resources.
Conclusion
Mpox is a rare but potentially serious viral disease that can affect both humans and animals. While it is less severe than smallpox, it still requires careful attention, especially in areas where the virus is endemic. By understanding the symptoms, transmission routes, and preventive measures, you can reduce your risk of contracting mpox and help prevent its spread. If you suspect you have been exposed to the virus or are showing symptoms, seek medical advice promptly to ensure proper diagnosis and care.
Although there is no specific treatment for MPOX, a combination of supportive care, antiviral medications, and preventive measures can effectively manage the disease and minimize its effects. Public health measures, including vaccination and surveillance, play an important role in controlling outbreaks and preventing serious consequences.
Ongoing research and improved access to antiviral treatments and vaccines will continue to enhance the management of MPOX in the future. Read More

Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Your article helped me a lot, is there any more related content? Thanks!
Your article helped me a lot, is there any more related content? Thanks!